ISSN electrónico: 1885-5210
DOI: https://doi.org/10.14201/rmc2020164261277
DIVE BOMBER (1941): A STUDY MODEL OF AVIATION PHYSIOLOGY
Bombarderos en picado (1941): un modelo de estudio de la fisiología de la aviación
Germán DOMÍNGUEZ-VÍAS
Departamento de Fisiología, Facultad de Ciencias de la Salud de Ceuta. Universidad de Granada (Spain).
E-mail address: germandv@ugr.es
Fecha de recepción: 4 February 2020
Fecha de aceptación: 25 February 2020
Fecha de publicación: 15 December 2020
Abstract
This article serves to begin in the teaching bases of the current aviation physiology, whose origin dates back to the beginning of World War II. Dive Bomber (1941) by Michael Curtiz is an excellent teaching material to help in the understanding of the different causes of the pilots’ syncope at heights, allowing thinking and the search for solutions or alternatives through experiments that allow the recovery of the body homeostasis. His audiovisual material shares real scenes of the United States Army that allow access to these discoveries and the progress of the current state of modern aerospace physiology.
Key words: altitude; hypobaric hypoxia; syncope; aviation.
Resumen
Este artículo sirve para iniciarse en las bases docentes de la actual fisiología de la aviación, cuyo origen se remonta al comienzo de la Segunda Guerra Mundial. Bombarderos en picado (1941) de Michael Curtiz es un excelente material docente para ayudar en la comprensión de las distintas causas del síncope de los pilotos en las alturas, permitiendo la reflexión y la búsqueda de soluciones o alternativas a través de experimentos que permiten la recuperación de la homeostasis corporal. Su material audiovisual comparte escenas reales del ejército americano que permiten acceder a estos descubrimientos y al avance del estado actual de la moderna fisiología aeroespacial.
Palabras clave: altitud; hipoxia hipobárica; síncope; aviación.
Technical details
Title: Dive Bomber.
Country: United States of America.
Year: 1941.
Director: Michael Curtiz.
Music: Max Steiner.
Cinematography: Bert Glennon, Winton C. Hoch.
Film Editing: George Amy.
Screenwriters: Frank Wead, Robert Buckner.
Cast: Errol Flynn, Fred MacMurray, Ralph Bellamy, Alexis Smith, Robert Armstrong, Regis Toomey, Allen Jenkins, Craig Stevens, Herbert Anderson, Moroni Olsen, Gig Young, Dennie Moore, Louis Jean Heydt, Cliff Nazarro.
Color: Color (Technicolor).
Runtime: 132 minutes.
Genres: Drama, War, World War II. Army. Based on real facts. Propaganda.
Language: English.
Production Companies: Warner Bros. Pictures.
Synopsis: History of a military flight surgeon doctor and a high-ranking pilot of the United States Navy who overcome personal differences to investigate the dizziness and fainting that pilots suffer when they fly high, in order to work on the solution of the problem of altitude sickness, developing a high-altitude suit that will protect pilots from fainting when they dive. Based on real events, it was released months before the Japanese attack on Pearl Harbor.
Awards: Academy Awards (USA): Oscar nomination for best color photography (Bert Glennon, 1942).
Link:
https://www.imdb.com/title/tt0033537/?ref_=ttawd_awd_tt
https://www.filmaffinity.com/es/film898574.html
International Trailer (original)
Introduction
Right at the beginning of the film it is specified that «this film is dedicated to the pioneering doctors of the air forces, in recognition of the heroic efforts to solve the complicated problems of aviation medicine». It is known that one of the greatest challenges of home-ostasis of human physiology was the ascension to increasing heights1. The human body is subjected to problems derived from the effects of the height itself and the low gas pressures, however, they pose greater challenges to an airplane pilot if we add, along with the great heights, the acceleration forces. The same is observed during dive bombing exercises starting at 600 meters above sea level (m.a.s.l.). During the 12th minute (12’:04’’), the maneuvers of downhill dive and subsequent correction in the trajectory affected the combat pilot initiating symptoms of discomfort and ending with loss of consciousness (syncope) and impact on the ground (Photo 1), being the common cause of spinal injuries and/or subsequent death due to elevated intracranial pressure during the surgical procedure.
American poster of Dive Bomber (1941).
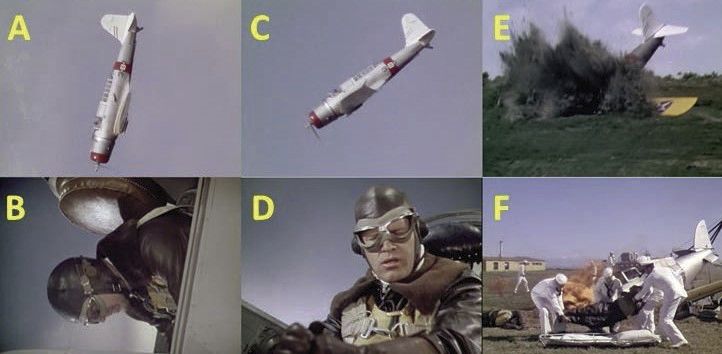
Photo 1. Dive exercise at 600 m.a.s.l. (A-B) and trajectory correction (C),
resulting in fainting (D) and fatal impact on the ground (E-F).
The first cervical vertebra (C1 or atlas) has the greatest mobility of the entire spine, and the joints between the occipital bone and the atlas (C0-C1) and between the atlas and the axis (C1-C2), anatomically very specialized, are biomechanically structured with a high range of mobility, in addition to being the osteoligamentous link between the head and the trunk. However, it makes them more vulnerable with greater likelihood of damage against numerous pathological processes2. Injuries to the C0-C1-C2 complex can cause muscle, ligament, joint or bone injuries; in many cases there are mixed lesions with a pejorative evolution and with the possibility of medullovascular involvement3,4, configuring the different types of dislocations or fractures of this complex (Photo 2). An elevated pressure in the spine, between the base of the skull and the atlas, can only be released if it is operated, despite the weakness of the patients and their loss of consciousness. Unnecessarily, these negative symptoms should appear on the cervical vertebrae just after the plane crashes. Cervical dislocations accompanied by hyperlordosis, fractures and/or death may even appear, for a fraction of a second, in the pilot’s work environment2, during the launch of the ejection seat, violent vibrations, or by the increase of G forces through accelerations and sharp turns5. The most relevant dislocations and trauma of the C0-C1-C2 complex are as detailed below.
Occipitoatloid dislocation
It is caused by the total rupture of the ligaments and joint capsules that join the atlas and odontoids to the occipital bone with the consequent dislocation of these, in high-speed accidents6. The traumatic separation between the atlas and the occipital bone in most cases is incompatible with life, since it can cause the section of the medulla or vertebral arteries. These lesions may be associated with fractures of the tip of the odontoid. Atlooccipital dislocation is a very unstable lesion that can cause distraction or compression of the spinal cord, brainstem or cranial nerves and vascular alterations due to stretching of the vertebral arteries. Clinically it can be manifested by paresis of nerves VI, X and XII cranial nerves, monoparesis, hemiparesis or tetraparesis, or respiratory dysfunction. It can also cause complete tetraplegia with apnea. They are injuries that have virtually no chance of spontaneous healing. Surgery by means of an occipitocervical instrumented fixation or, occasionally, a posterior atlooccipital interarticular fixation7,8 achieves proper alignment and stabilization of dislocation and thus prevents the onset or worsening of the neurological clinic.
Atlas Fractures
They represent 4-15% of all cervical spine fractures and 1-3% of all spinal fractures. 39-56% are presented as isolated fractures and in 50% of cases they are associated with axis fractures. Given the special anatomical configuration of the atlas, trauma to this vertebra can produce a considerable combination of lesions on the masses or the anterior, posterior and/or lateral arches of this vertebra (Photo 2), injuries already classified by Jefferson9 in 1920. Patients with isolated fractures of the atlas who arrive at the hospital almost never have neurological symptoms. There is little data to suspect an atlas fracture in traumatic patients who arrive at the hospital unconscious. In lucid patients, the mechanism of the accident, together with the presence of cervical contracture and pain, limitation of head movements, suboccipital pain, or occipital anesthesia or neuralgia can guide the diagnosis. The presence of a retropharyngeal hematoma can be suspected in the presence of dysphagia or dysarthria.
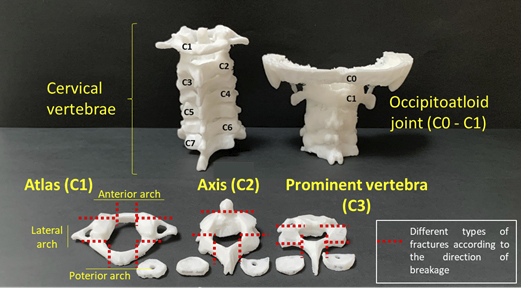
Photo 2. 3D printed replicas of the skull base (occipital bone or C0) that articulates with the
first cervical vertebra (C1 or atlas) and this in turn with the second cervical vertebra (C2 or axis).
All possible unilateral or bilateral fractures of each vertebral arch are shown in red.
Axis fractures
They represent up to 17% of all cervical fractures. Of these, 55% are fractures of the odontoid process, 23% are fractures of the pedicles and 22% settle in the body of the axis or in other less frequent locations.
Fractures of the odontoid process (OP)
It is the most frequent type of fracture of the upper cervical spine. The fracture of the odontoid base is tremendously unstable and with enormous evolutionary danger if consolidation is not achieved. The vast majority of patients arriving with odontoid (OP) fractures are neurologically unscathed10,11. However, it is a type of fracture that can cause death from spinal shear or serious neurological injuries at the time of the accident3,12. Clinical cervical myelopathy may appear in weeks, months or even years after the fracture occurs13,14. Those neurologically asymptomatic patients who with a correct treatment achieve the reduction, fixation and bone fusion of their fracture, get the cure of these serious injuries10.
The rupture of the isthmus (also known as pars interarticularis) of the axis favors spondylolysis, so that the joint process is separated from the vertebral body15. Fractures that settle in the posterior elements of the second cervical vertebra are also known as the fracture of the «pars interarticularis», traumatic axis spondylolis- thesis or Hangman’s fracture. It is a type of fracture that, in its greatest expressiveness, occurs in prisoners sentenced to hanging, a fracture that in these cases is associated with a brutal dislocation C2-C3 by a mechanism of hyperextension-distraction. It can also be presented by a hyperextension-compression mechanism in traffic accidents or falls, similar to hanged men. The objective in Hangman’s fractures caused by hanging is the death of the inmate by spinal shear and vertebral arteries. As a complication of spondylolysis, and a frequent cause of pain, spondylolisthesis or sliding of one vertebra over another appears.
Atloaxoid associated fractures and dislocations
The existence of fractures16 and dislocations17 combined atlas and axis is relatively frequent, as well as evident in fighter plane pilots and helicopters18. From the anatomophysiopathological point of view and of the harmful mechanisms of clinical biomechanics, very important pathomechanical forces are required for the production of these lesions that normally imply the coexistence of a greater number of neurological deficits (12%) than in the case of fractures isolated from the atlas (0%) or the axis (2%). The combination of atlas and axis fractures occurs in 15% of odontoid fractures and in 9% of pedicle axis fractures3,4. Numerous possibilities of combinations have been described, but the most frequent are: fractures of the atlas and the base of the odontoid process (40%), atlas fractures and fractures of the axis body (28%), atlas and transverse fractures of axis (20%), fractures of the atlas and pedicles of the axis (12%) or fractures of the odontoid process associated with rupture of the transverse ligament of the atlas3,4. The vast majority of these fractures are unstable.
Syncopes
In the middle of the Second World War, fainting in dive bombers were interesting for both US Army and German doctors. The flight at more than 9,000 m.a.s.l. supposed deaths due to crashing without apparent causes, attributed to altitude sickness with loss of consciousness, dizziness from hypobaric hypoxia and hypothermia1. Moments after the war, they discovered that exposure to high sustained acceleration (+G or load of inertia from head to toe) has harmful effects on the body of pilots in flight, creating forces acting on a pilot between five to ten times stronger than gravity. The most important effect of centrifugal acceleration (+G or force G) on the body occurs at the level of the circulatory system19, because the blood is mobile and can be displaced by centrifugal forces. An aviator sitting in the seat of his cockpit, the force with which he compresses the seat is due to the force of gravity and is equal to its weight (+1 G). If the force with which the seat is compressed becomes five times its normal weight during the exit of a dive, the force that is subjected on the seat is greater (+5 G), the blood moving from the upper body towards the vessels of the lower part of the body, dilating passively until reaching a venous pressure of ~300 mmHg (or ~50 mmHg if it remains standing and motion-less). At the beginning of the acceleration, the effect of the force G (+4 G/+6 G) on a pilot occurs with visual loss (black veil) and consciousness due to a deficit of cerebral perfusion pressure (PPC or blood pressure necessary to perfuse the nervous tissue for a good metabolic functioning). Since the heart cannot pump unless blood returns to its interior, the greater the amount of blood that stagnates in the lower part of the body, the lower the amount of blood available for cardiac output. Both systolic and diastolic pressure decrease well below nor- mal (PS and PD: <22 mmHg) at the beginning of the first seconds of acceleration (+3.3 G), but in response to the loss of homeostasis, a baroreceptor reflex is then activated quickly to help restore these pressures a little (PD: ~55 mmHg; PD: ~20 mmHg). Accelerations greater than +4 G to +6 G occurring in a time range after blindness and unconsciousness are dangerous because of increa- sing lethality range. Other clinical data that occur in pilots, and whose precise cause remains undefined, is the presence of changes in the electrical waves of the heart20 and liver dysfunction with morphology and metabolic activity21.
This film recounts all the experimentation carried out until the discovery of the cause of fainting and the prevention of loss of irrigation in the brain. In the 21st minute (21’:30’’), one of the first options they considered for the fight against syncope was to reduce the speed of the dive with the flaps (surfaces that are on the wings that allow to increase the lift of the aircraft by reducing speed in takeoff and landing maneuvers). As the results were not as expected, from the 33rd minute (33’:40’’), the practical exercises for the pilot’s aviator training of the pilot’s flight book are described, performing (Photo 3): (a) spirals, (b) landings, (c) acrobatics, (d) turns, (e) rapid recovery (plummeting, turning, until straightening the plane), (f) hypobaric chamber experiments for the study of oxyhemoglobin dissociation curves, in relation to the partial pressure of oxygen (PO2) and the oxygen saturation to hemoglobin, and the effects of the partial pressure of carbon dioxide (PCO2), pH and temperature on the oxygen dissociation curve (Bohr effect). These types of hypobaric chambers are widely used for the training of military pilots, simulating cabin decompression and hypoxia of great heights22. A pilot who breathes air in an unpressurized aircraft cannot ascend to heights much greater than one who breathes pure oxygen, being able to remain conscious until the arterial oxygen saturation decreases to the ceiling of 50% (~7,000 m.a.s.l.). Oxygen saturation in the hemoglobin of arterial blood when breathing pure oxygen remains above 90% until the pilot rises to 12,000 m.a.s.l., so depressurization at this height would cause extreme hypoxia and loss of consciousness, being automatically correctable with the use of masks that supply 100% oxygen that, while descending the plane, protect from hypobaric hypoxia. Above 12,000 m.a.s.l. Oxygen saturation decreases rapidly to approximately 50% (~14,300 m.a.s.l.). Other models of more modern fighter jets, such as supersonic airplanes, make flights above 12,000 m.a.s.l., where depressurization at that height causes a rapid loss of consciousness, forcing the permanent use of breathing equipment to safety. pressure that supplies oxygen at 40 cmH2023.
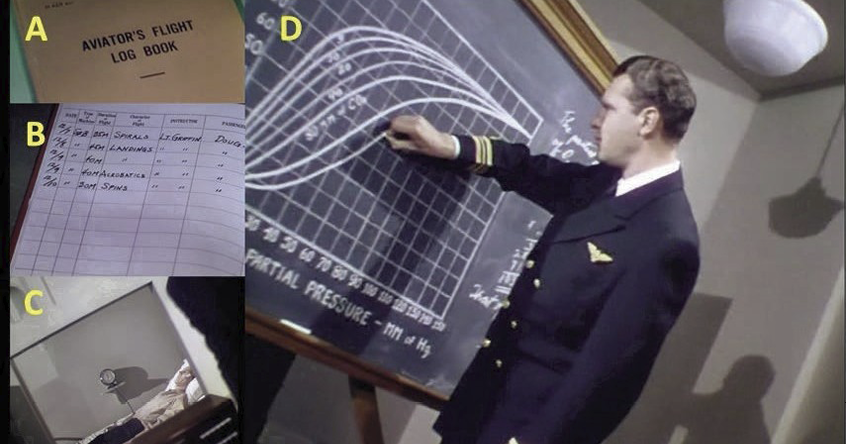
Photo 3. Practical exercises for aviator training listed in the pilot’s flight book (A-B), hypobaric exercise test (C) and measurement of the hemoglobin dissociation curve by the Bohr effect (D).
The use of recording instruments and a film camera on the plane was an advance to test and record previous movements that prevented or favored the unconscious delay. From minute 52 (52’:00’’), doctor and pilot replicate together (a) plummets, (b) speed tunnel tests, and (c) traced to +9 G, with indications of the trial instructor asking that in the first comeback the muscles of the head to the feet are tightened, tightening the belly to the maximum and shouting with all the forces to verify if this action avoids the fading. The recordings indicated that shouting was of no use when it was traced after performing a chop at different stabilized heights (4,500 m.a.s.l. - 1,500 m.a.s.l.). In any case, the fainting was milder and woke up in seconds, but it was not effective (Photo 4). Chance wanted the flight doctor not to faint by changing his postural position after leaning to fix the camera jam immediately after the comeback. The doctor was at that time inclined with the heart at the level of the brain and the blood was at the level of the heart, avoiding fainting, but did not prevent the appearance of dizziness. This is currently a body protection technique against circulatory collapse that could occur during G+. If the aviator tenses the abdominal muscles to an extreme degree and leans forward to compress the abdomen, part of the accumulation of blood in the large vessels of the abdomen can be avoided, thereby delaying the onset of pilot syncope24.
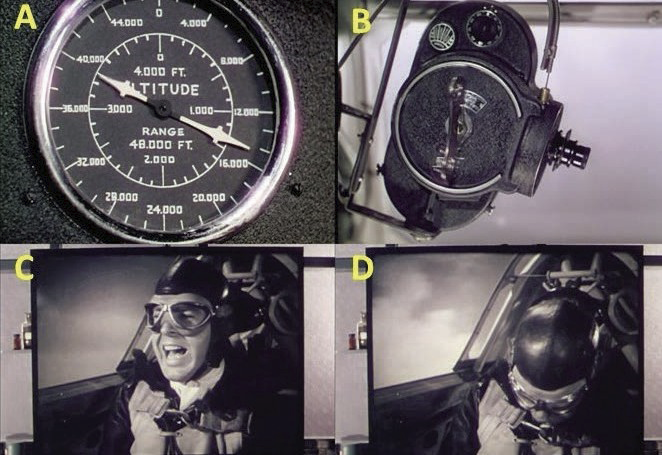
Photo 4. The images recorded inside the cockpit showed that shouting during the comeback,
at 4,500 m.a.s.l. (14,763.76 feet) after a dive, did not prevent fainting.
In the 1940s, Dr. Wilbur Franks invented the first anti-G suit, called Frank’s flight suit, being the first model that prevented the loss of consciousness by G forces (G-LOC), up to +9 G in modern combat suits, acting directly on the prevention and/or treatment of orthostatic hypotension25. In the film that moment is reflected in the 60th minute (60‘:17’‘), where the birth of that same suit arises from the joking joke of a pilot, ensuring that a hard neck that drowned the pilot would prevent the blood from coming down from the brain. Just then they get the use of a pneumatic belt, as a corset, that at the start of the dive it will inflate and press the stomach, under the ribs, compressing the entire abdominal region and favoring the blood to remain above the heart (Photo 5, A-D). Then (61’:21’’) the doctor successfully tests the experimental suit, hooking a compressed air from the cabin to the corset. At the moment of the start of the dive the pilot opens the valve and the suit is inflated, helping the compression of the blood vessels. At the exit of the dive, no dizziness or syncope was observed (Photo 5, E and F). This test solved the problems of fainting and the authorization of these belt models was approved by Washington.
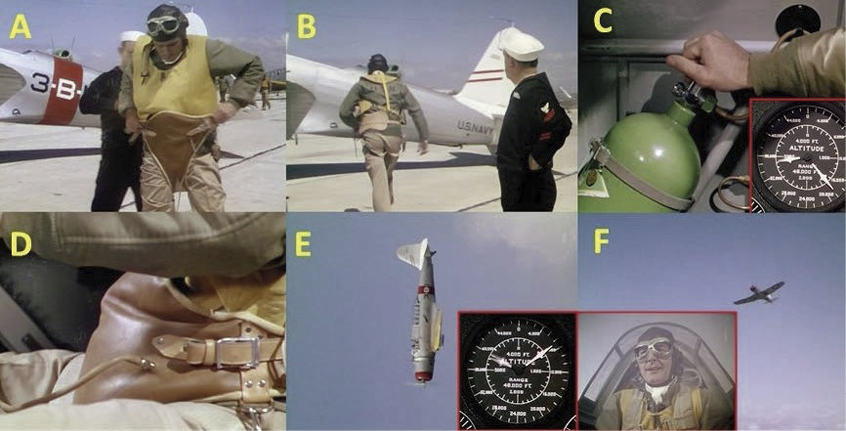
Photo 5. (A-B) Test test of the first anti-G suit during a dive flight. (C-D) A ~5,791 m.a.s.l. (~19,000 feet)
the chopping begins and the compressed air valve opens to inflate the pneumatic belt. (E-F)
During the comeback at ~2,438 m.a.s.l. (~8,000 feet), you can avoid fainting.
Attention capacity and physical fitness
For the study of cognitive processes that affect attention, a series of tests are performed that measure and improve the amount of concentrated time that a person can devote to a task without being distracted. One of the exercises is done with airplane simulators to fly blind flights. During the 40th minute (40’:18’’), one of the indications of the medical instructor is not to rely on the senses but on the flight instruments, because the auditory ducts give a deceptive sense of orientation (Photo 6). Later (45’:17’’), it is proposed to use the Rorschach test (analysis of ink spots) to determine personality characteristics (psychological problem and psychic state) and emotional functioning (mood and fatigue) of the aviation personnel through a series of projective tests26-28. All those pilots who did not pass the psychological tests were removed from their services for presenting temporary stages of mental alienation, an incorrect term that changed its name in the 90s after the Vietnam War, becoming called posttraumatic stress29,30. Other complementary tests that are carried out are those of orientation and dizziness reaction (58’:18’’), placing the pilot on a swivel chair and the doctor activates a crank that activates a rotation mechanism on its same axis (Photo 6).
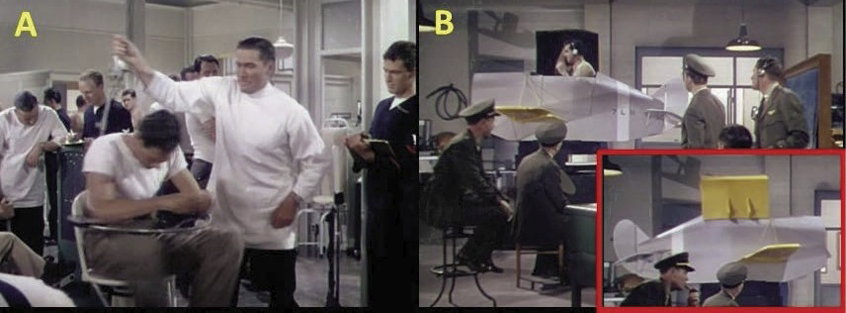
Photo 6. Dizziness (A) and attention (B) tests of the flight simulator.
Along with the previous tests, new tests are carried out that determine if the pilot can continue flying through the detection of changes in pulsations and blood pressure. Among them is the cardiovascular assessment system or Schneider test31. Schneider described a method to assess physical fitness in 1920, using six sets of observations: (a) pulse rate in the reclined position; (b) foot pulse rate; (c) the increase in pulse rate when foot and recline frequencies are compared; (d) the increase in pulse rate after standard exercise; (e) the time required for the heart rate to return to the heart rate after exercise; and (f) the change in systolic blood pressure when the examinee stands up. This test is used as a general indication of physical fitness and to give an idea of the ability of the heart to adapt to a greater requirement of the circulatory system, thus certifying the presence or absence of «pilot fatigue». In the 70th minute (70’:10’’), one of the doctors from the San Diego military base (USA) forbids one of his pilots to fly due to the chronicity of fatigue. The doctor points out the unfavorable evolution of his graph (in red), showing the decisive points of irritability, stress and low form, so he recommends stop flying for a long time (2 months) or even never (Photo 7).
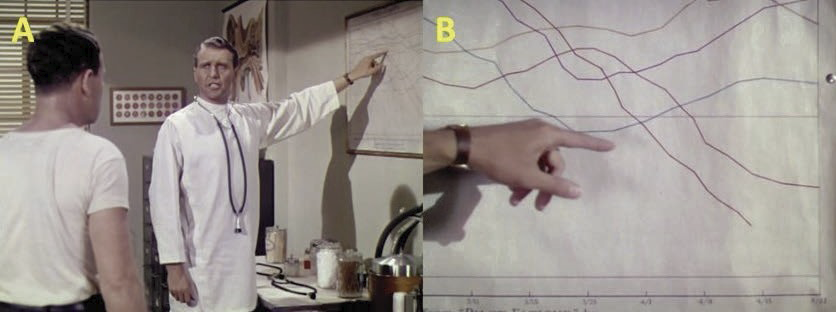
Photo 7. Schneider index graph in a case of a pilot presenting the critical point of the «pilot fatigue» line.
Hypobarism
The use of the pneumatic belt proved to avoid fainting, but caused other consequences due to altitude, hypoxia and nitrogen decompression at heights at 7,000 m.a.s.l. Studying how to get a denitrogenated pilot on the plane was an almost impossible cause, but it was possible to reproduce and evaluate low pressure flight conditions at high altitudes with the help of a hypobaric cabin. The activation of a pump (Photo 8A) to extract the air and decrease the atmospheric pressure inside a chamber with animals and/or humans (Photo 8, B and D-I), facilitated the simulation of these environmental conditions in relation to altitude, up to 12,000 m.a.s.l. as limit (Photo 8, C and E). The adjustment of oximeters to the ear helped to monitor how much oxygen is in the blood (Photo 8G). At higher altitude, greater clumsiness to coordinate flight maneuvers properly. This is shown by an exercise (75’:00’’) where pilots must follow the movement of a light on a panel, with the help of the controls as they ascend (Photo 8H). A green light shows the ability to coordinate. Listed below are all the increasing intervals to which they were subjected (in m.a.s.l.): 1,500, 1,800, 2,100, 2,400, 2,700, 3,000, 3,300, 3,600 (a group of test pilots are placed on the oxygen masks; Photo 8I), 3,900, 4,800, 5,700, 6,000, 6,400 (hypobaric hypoxia effects appear in pilots who decided not to put on the oxygen mask; Photo 9A), 6,700 (unfocused vision of the lights and loss of coordination. Needle drop to the red zone below 50% of the oxygen saturation ceiling in arterial blood, with imminent fainting. The implementation of oxygen therapy leaves the red zone and quickly restores oxygen saturation in arterial blood above 50%; Photo 9, B-E), 7,300, 7,600, 8,200, 8,500, 8,800, 9,000, 9,300, 9,600 (presence of hypoxia with cyanotic faces, the needle drops 60% sharply; Photo 9F), 10,600 (maximum opening of the valve oxygen and cyanosis disappears. They reason that the cause of this problem is due to a miscalculation, as it is poorly adjusted for a person of his complexion), 10,900, 11,200, ~12,000 (auscultate heart sounds; Photo 9G). Being all cyanotic, they notice that their heart rates are much slower than that of a person with enough oxygen), 12,000, end of the test. At 12,000 m.a.s.l. they stop ascension and study how long they are able to withstand this pressure, observing everyone suffering from hypoxia and hypoxemia (saturation values well below 50%). After the test, reduce the height (increase the pressure) suddenly and be aware of being careful with the ears. In the 90th minute (90’:50’’), one of the pilots manifests an embolism in the knee region (Photo 9H). The doctor massaged the painful area and rubbed hard to reactivate blood flow, indicating as if in his circulation he had gelatin. Radiological tests on elbow and knee joints (Photo 9, I-J) showed evidence of bubble formation only in the knees. The evidence strongly related that, at higher altitude, more sudden decompression sickness problems occurred, with the only therapy being the use of hyperbaric chambers32-34. This decompression sickness with the decrease in barometric pressure causes the formation of bubbles in situ from dissolved inert gas and arterial gas embolism, in which the alveolar gas or the embolism of venous gas (through shunts or bypassing vessels pulmonary) are introduced into the arterial circulation35.
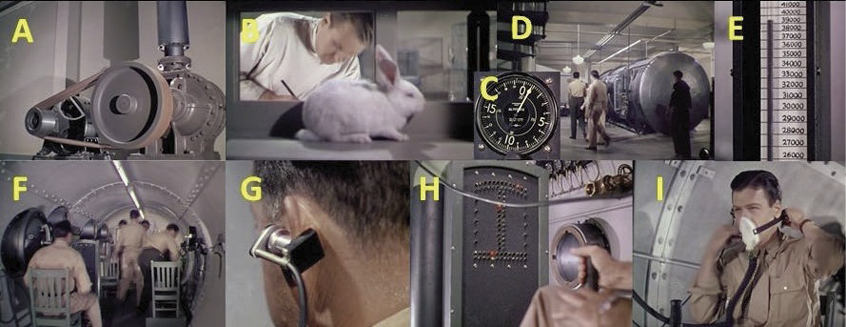
Photo 8. Experiments of hypobaric hypoxia in animals (B) and humans (D-I) with the purpose of studying
how the lack of oxygen affects the ability to coordinate movements. A pump extracts the air (A)
from the chamber to simulate the conditions of low atmospheric pressure in the ascent,
until reaching 12,000 m.a.s.l. (39,370 feet; E).
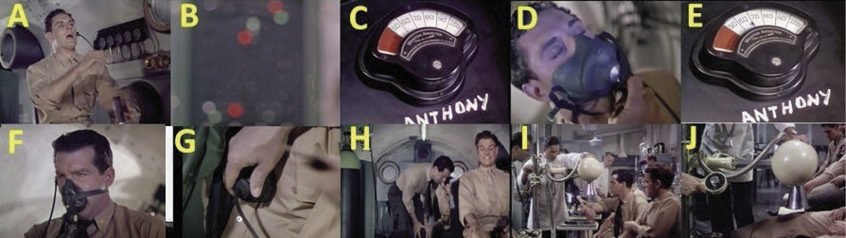
Photo 9. (A-C) Below the ceiling of arterial blood oxygen saturation (<50%), the pilot loses consciousness. (D-E) Oxygen therapy restores the recovery of knowledge and oxygen saturation in hemoglobin above 50%. (F-G)
The effects of cyanosis slow the heart rate. (H-J) Radiological tests show that at higher elevations it can favor the appearance of emboli due to the disease of decompression in the joints.
To avoid decompression sickness, discuss (91’:56’’) the possibility of restricting flights to 10,600 m.a.s.l. being the limit, but the military rebut that an allied fighter must get over other enemy fighters without restricting altitude. That is why they begin to study a new objective, find the causes of dizziness at high altitudes and check if it is due to lack of oxygen or bubble formation. It was known that pilots needed oxygen above 3,600 m.a.s.l. and they did not know the causes that caused the dizziness, but how to avoid them making the pilots always at the same pressure as at sea level (760 mmHg)1 no matter how much the pilots climb with the help of pressurized cabins. In addition, the weight of a pressurized cabin would make it rise 1,500 m.a.s.l. less in a fighter, being ideal for large airplanes where the weight does not matter so much.
To alleviate these depressurization health problems, the use of pressurized cabins or the need for a pressurized suit (92’:33’’) was raised, so that they are always at the same pressure as at sea level, without analogies to an armor because of the difficulty that the movement would entail. In addition, the suit should have flexible joints, with some similarity to the design of scuba divers’ suits, and with the ability to retain oxygen inside. However, the experimental test with the pressurized cabin was a failure and almost caused the death of the protagonists. The cabin had valves that regulated oxygen, temperature and barometric pressure within the entire aircraft, but it was not thought that, at 10,600 m.a.s.l., due to the effect of hypothermia associated with height, moisture would condense (photo 10C) and they would freeze the regulators of the valves (photo 10, A-D), not being able to balance per se neither the temperature, nor the humidity, and freezing the antifreeze and the controls of control, making it impossible to ice the flight leaving it unanswered and completely unusable. All this, together with hypobaric hypoxia, caused a cyanosis picture followed by the syncope of one of the pilots. The doctor’s rapid intervention at the controls of the plane and his assistance with oxygen masks prevented them from crashing.
The unsuccessful previous result resulted in experimenting with pressurized armor, whose design resembles modern aerospace suits (Photo 10, E and F). The suit test is fully functional in the hypobaric chamber after simulating higher heights of 12,000 m.a.s.l. (112’:31’’), stopping the test at 13,700 m.a.s.l. The actual test inside an airplane showed that the suit was fully functional (Photo 10G). From 10,000 m.a.s.l. the suit worked correctly and the regulation of more oxygen was viable, despite finding signs of freezing in the oxygen regulating valves and altimeter, to which the pilot warns, before dying, that future improvements to the suit should be added as mechanisms that will heat the oxygen tube to avoid ice; in this way perfection would be achieved in the pressurized suit (Photo 10, G-L). It is likely that the cause of this syncope is, as with diver suits, poor ventilation due to the deficit of PO2 and the accumulation of accumulated carbon dioxide levels, causing hypoxia and drowsiness effects. At the end of the movie it is shown how the improved version of this suit was evaluated on a flight with test pilots and approved by the US Army.
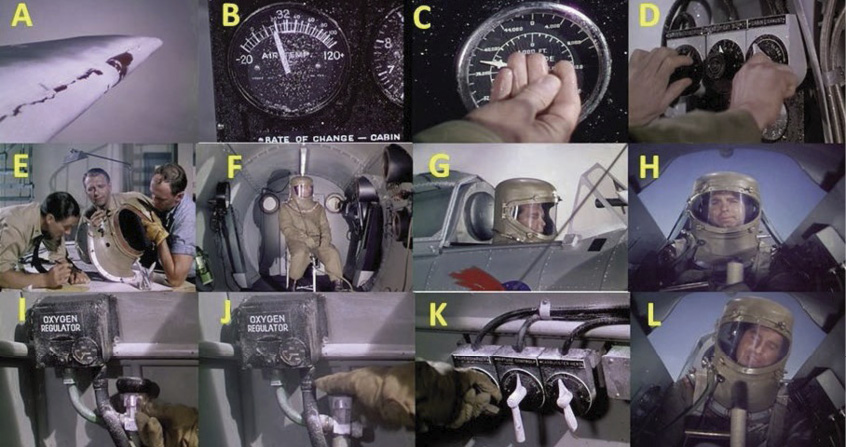
Photo 10. (A-D) The tests with a pressurized aircraft was a failure to freeze the steering and all
the equipment, causing syncope in one of the pilots. (E-F) Design of a pressurized suit
and test in hypobaric chamber. (G-L) Actual test of the pressurized suit being functional,
but with a fatal outcome for the pilot for freezing the oxygen regulator.
Results and Discussion
This work details one of the most accurate films in the description of the physiological alterations produced by a hypobaric environment. During the World War II contest, the test pilots sought to achieve, against the clock, countermeasures that prevented the death of more pilots because of the harshness of the physical environment than the battle itself5,12. The study of physiology in special situations to recover body home-ostasis was a great challenge, and it was known that solving that problem would give an advantage to win the war. Today these feats have already become almost routine, and physiological behavior is better known when the body adapts to adverse conditions. For an aviator, physiological changes are important due to differences in pressure and the amount of ambient oxygen, in extreme temperatures and also, in the case of maneuvers with turns, stunts and dives, due to acceleration and weightlessness19,22,34.
This film as an audiovisual model is interesting for providing data that would complement the teaching-learning on the syllabus of (a) anatomy by severe trauma after crashing for syncope, and (b) physiology at great heights and aeronautical flights, offering a large amount of simulated details of medical problems related to altitude exposure, as a determinant of altitude factors, speed (ascent / descent) and duration of exposure. It is also observable in the film that other factors not related to height, level of exercise developed (physical tests), psychological behavior, individual physiological susceptibility, in addition to the age of the pilot offered to the tests are considered. The reason that test pilots have different behaviors within the hypobaric chamber is a function of all these factors, varying in frequency of occurrence (from rare to common) and in intensity using line graphs that delimit whether they are benign and self-limited or they evolve rapidly until they become a fatigue, making it impossible for the pilot to continue the tests until his recovery (in case it is reversible). All these alterations and states of stress, or a continuous accumulation of these factors, are caused by altitude sickness (acute altitude sickness), giving rise to altitude edemas induced by hypoxia1, specifically the appearance of pulmonary edema, cerebral edema and/or peripheral edema. Many of the pilots who ascend to high altitude presented ventilatory changes22, cardiovascular in your blood pressure, heart rate, and in the electrical signal of the heart20,24, in addition to hepatic functional changes and other metabolic alterations21. On the one hand, the induction of hypoxia seems to be related to the appearance of these edema due to sodium and water retention1. It can also occur due to decompression thromboembolic problems, ischemic accidents, deep vein thrombosis, hypoxia-induced polycythemia, coagulation abnormalities, dehydration, freezing, and/or venous stasis for prolonged periods of sitting during long flight hours36,37.
The medical tests performed on the pilots of this film take place at the same height as the current commercial flights, between 9,000 - 12,000 m.a.s.l., with the advantages of saving fuel and having greater climatic stability at that point. At that time it was still unusual to use airplanes with pressurized cabins and suits. An experimental model that they develop in the feature film, to avoid fainting at heights, is just the test of one of those booths. Despite not giving a positive result in the experimentation, currently all commercial aircraft models have developed, and improved, that system, so the cabin must be pressurized with internal pressures equivalent to those at altitudes below 2,400 meters above sea level, what is called «cabin altitude». The difference in pressure between the exterior and the interior is not constant, in practice, and increases as the plane rises at a higher altitude. Typically, the cabin altitude does not exceed 2,000 m.a.s.l., which corresponds to pressures greater than 600 mmHg and a percentage of oxygen equivalent to sea level. Under physiological conditions, these values cause a slight decrease in oxygen saturation and minimal physiological changes. However, it can be dangerous for patients with respiratory failure who have a PO2 below 70 mmHg, unless they are treated with supplemental oxygen38,39.
A very successful aspect of this film is the phenomenon of gravity from the point of view of physiology, characterizing the characters that reach G+ of considerable magnitudes during the dives, considering positive the forces that press the individual against the seat and blood towards the feet, causing temporary blindness and even long-term injuries, significantly affecting this mobile characteristic of blood by centrifugal forces to the lower part of the body, increasing the hydrostatic pressure in the veins of the feet (with appearance of edemas), a decrease in venous return and, therefore, in cardiac output, resulting in arterial hypotension, dizziness, loss of consciousness, and even death or fractures and spinal injuries if acceleration persists. The development of anti-gravitational or anti-G suits was a great achievement in the film and in reality, decreasing the displacement of blood by pneumatic compression, as accelerations increase, towards the lower areas and avoiding the accumulation of blood In leg and abdomen.
Conclusions
Dive bomber is a teaching resource for teachers who want to convey in a very good way concepts of environmental adaptation in aviation physiology. All clinical and experimental cases of the film are based on real events and reliably relate the route of the scientific method to give answers to all the unknowns that triggered the crashing of the plane and the death or paraplegia of the pilot due to anatomical alterations.
Acknowledgment
Dr. Domínguez-Vías thanks Professor Dr. José Juan Vallo de Castro, from the physiology area of the University of Cádiz, for sowing the valuable seed of knowledge in aviation physiology.
References
2. Shin YH, Yun C, Han AH. Cervical spine status of pilots and air-controllers of air-borne early warning and control aircraft. Aerosp Med Hum Perform. 2017;88(5):476-80.
6. Wiegmann DA, Taneja N. Analysis of injuries among pilots involved in fatal general aviation airplane accidents. Accid Anal Prev. 2003;35(4):571-7.
7. Gonzalez L. Technique for fixating the atlantooccipital complex with a transarticular screw. Spine (Phila Pa 1976). 2002;27:219-20.
8. Grob D. Transarticular Screw Fixation for Atlanto-Occipital Dislocation. Spine (Phila Pa 1976). 2001;26(6):703-7.
9. Jefferson G. Fracture of the atlas vertebra. Report of four cases, and a review of those previously recorded. Br J Surg. 1919;7(27):407-22.
10. Martin-Ferrer S, Rimbau J, Joly MC, Teruel J, Pont J. Fracturas de la apofisis odontoides: Revision de nuestra casuistica, implicaciones terapeuticas y nueva clasificacion. Neurocirugia. 1999;10(6):426-38.
11. Martín Ferrer S, Rimbau Muñoz J, Feliu Tatay R. Atornillado anterior en las fracturas agudas de la odontoides. Neurocirugia. 1996;7(2):89-99.
12. Adams VI. Neck Injuries: II. Atlantoaxial Dislocation. A Pathologic Study of 14 Traffic Fatalities. J Forensic Sci. 1992;37(2):13263J.
13. Bachs A, Barraquer-Bordas L, Barraquer-Ferré L, Canadell J, Modolell A. Delayed myelopathy following atlanto-axial dislocation by separated odontoid proces. Brain. 1958;78(4):537-53.
14. Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: Clinical, radiological, and surgical features. J Neurosurg. 1993;78(4):579-86.
16. Hadley M, Walters B, Grabb P, Oyesiku N, Przybylski G, Resnick D, et al. Management of Combination Fractures of the Atlas and Axis in Adults. Neurosurgery. 2002;50(suppl_3):S140-7.
17. Yoon DH, Yang KH, Kim KN, Oh SH. Posterior atlantoaxial dislocation without fracture: Case report. J Neurosurg. 2003;98(1 Suppl):73-6.
18. Tolga Aydoğ S, Türbedar E, Demi˙rel AH, Teti˙k O, Akin A, Doral MN. Cervical and Lumbar Spinal Changes Diagnosed in Four-View Radiographs of 732 Military Pilots. Aviat Space Environ Med. 2004;75(2):154-7.
19. Scott JM, Esch BTA, Goodman LS, Bredin SSD, Haykowsky MJ, Warburton DE. Cardiovascular consequences of high-performance aircraft maneuvers: Implications for effective countermeasures and laboratory-based simulations. Appl Physiol Nutr Metab. 2007;32(2):332-9.
20. Comens P, Reed D, Mette M. Physiologic responses of pilots flying high-per- formance aircraft. Aviat Space Environ Med. 1987;58(3):205-10.
26. Guerrier S. Man on the moon. The Lancet Psychiatry 2019;6(7):570-2.
28. Shayler DJ, Burgess C. The selections, Chapter 1. In: Shayler DJ, Burgess C, editors. The Last of NASA’s Original Pilot Astronauts: Expanding the Space Frontier in the Late Sixties. Cham, Switzerland: Springer International Publishing AG; 2017. p. 1-31.
30. Schlenger WE, Kulka RA, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. The prevalence of post-traumatic stress disorder in the Vietnam generation: A multimethod, multisource assessment of psychiatric disorder. J Trauma Stress. 1992;5(3):333-63.
32. Jain KK. Cerebral Air Embolism, Chapter 12. In: Jain KK, editor. Textbook of Hyperbaric Medicine. 6th ed. Cham, Switzerland: Springer International Publishing AG; 2017. p. 121-30.
33. James PB, Jain KK. Decompression Sickness, Chapter 11. In: Jain KK, editor. Textbook of Hyperbaric Medicine. 6th ed. Cham, Switzerland: Springer International Publishing AG; 2017. p. 101-20.
34. Gentry J, Rango J, Zhang J, Biedermann S. Latent presentation of decompression sickness after altitude chamber training in an active duty flier. Aerosp Med Hum Perform. 2017;88(4):427-30.
35. Tawar A, Gokulakrishnan P. Decompression illness. J Mar Med Soc. 2019;21(2):112.
36. Smith TG, Chang RW, Robbins PA, Dorrington KL. Commercial air travel and in-flight pulmonary hypertension. Aviat Space Environ Med. 2013;84(1):65-7.
37. Schreijer A, Cannegieter S, Caramella M, Meijers J, Krediet R, Simons R, et al. Fluid loss does not explain coagulation activation during air travel. Thromb Haemost. 2008; 99(06):1053-9.
|
|
German Dominguez Vías. Doctor of Medicine from the University of Cádiz. Master’s Degree in Advances in Food Safety and Bachelor of Biology from the University of Jaén. He is currently an assistant professor doctor of the Faculty of Health Sciences of Ceuta of the University of Granada, where he teaches associated with the department of physiology in the nursing degree, and implements the Cinema as an educational resource within the curriculum. His line of research focuses on neurodegeneration and blood pressure regulation. |
